⏱ 3 Min Read
What is endometrial hyperplasia and is it serious?
Written by
Eleni Stefanou
Medically reviewed by
Dr Dupe Burgess, BSc, MBBS, MRCP
Updated on
4 Apr 2024
📋 In this guide
What is endometrial hyperplasia?⟶
How common is it? ⟶
What are the symptoms of endometrial hyperplasia? ⟶
What causes endometrial hyperplasia? ⟶
What drives the hormone imbalance behind endometrial hyperplasia? ⟶
Is endometrial hyperplasia a serious condition? ⟶
How is endometrial hyperplasia diagnosed? ⟶
How is endometrial hyperplasia treated? ⟶
Specialists to speak to ⟶
4 parting tips ⟶
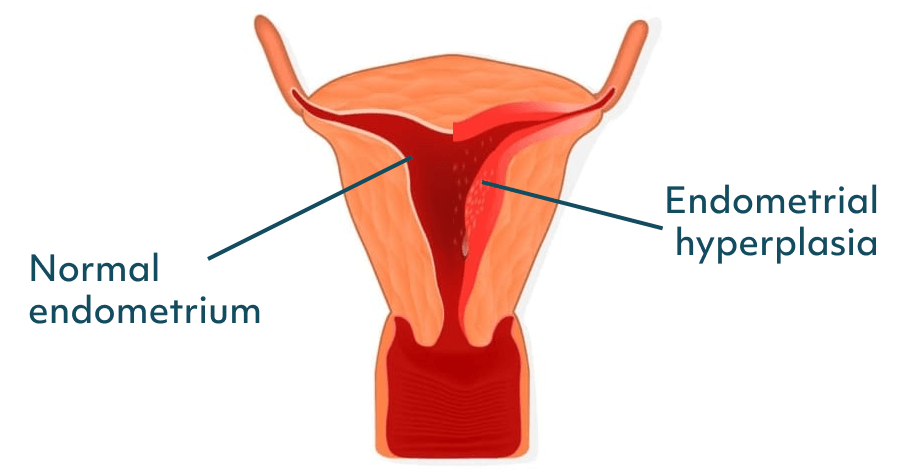
Let's start with the basics: the endometrium is the layer of tissue that lines the uterus. This tissue thickens each month in preparation for a potential pregnancy and its top layer sheds during your period. Sometimes this tissue can become too thick, leading to endometrial hyperplasia. Hyperplasia is when increased cell production occurs in a normal tissue or organ.
It’s pretty rare. Research suggests that about 133 in 100,000 women will develop endometrial hyperplasia. It’s most common in women aged 50–54 and is rarer in women under 30. (1)
If you notice any of these symptoms, book an appointment with your healthcare provider, especially if they’ve lasted for more than three months:
Heavy or prolonged periods
Bleeding between periods
Changes in menstrual patterns (eg shorter or longer cycles than usual)
Bleeding after menopause
Pelvic pain, pressure or cramping
Anaemia and associated symptoms (eg fatigue, weakness, shortness of breath)
An imbalance between the hormones oestrogen and progesterone can lead to hyperplasia. If you have too much oestrogen and a deficiency in progesterone over a long period, your uterine lining can thicken excessively. (2)
You have a higher likelihood of developing endometrial hyperplasia if:
You are 35 or older
Have never had children
Are in perimenopause (the transitional time before menopause)
Have already reached menopause or are postmenopausal
Started your periods before you were 12
Were 55 or older when you reached menopause
Have diabetes
Have a family history of uterine, ovarian or bowel cancer
Factors that can lead to an oestrogen and progesterone imbalance include:
Obesity (fat tissue can convert other hormones into oestrogen leading to excess levels)
Hormone Replacement Therapy (HRT) with no or too little progesterone
Certain medications that can act like oestrogen (eg tamoxifen)
An ovarian tumour that excretes oestrogen
It depends on the type of hyperplasia. Atypical endometrial hyperplasia is when the cells are abnormal. In this scenario, there is a higher risk of these cells developing into cancer. Endometrial hyperplasia without atypia is when the cell structure is normal.
In both cases ongoing monitoring is important and your risk of developing cancer will be measured alongside other factors.
The good news is that most women won’t develop cancer from endometrial hyperplasia and treatment of the condition has a high success rate.
Pelvic exam and transvaginal ultrasound
These are usually the first steps in examining whether your endometrium is abnormally thick.
Biopsy
A small cell sample from the endometrium is taken and examined under a microscope.
Hysteroscopy
This is where a small camera is placed inside the uterus to assess the endometrium. A biopsy may be taken at the same time.
If you have endometrial hyperplasia without atypia (cell structure is normal) then the most common treatment options are:
Progesterone treatment
You may be given a synthetic form of progesterone as a tablet or as a hormone-releasing coil (Mirena intrauterine system). The coil has the highest success rate when it comes to treating endometrial hyperplasia and the least side effects. Overall, there is an 89-96% chance that your endometrium will return to normal with a progesterone treatment. (3)
Watch and wait
You and your healthcare provider may choose to monitor whether the uterine lining returns to normal without treatment. If you have risk factors (eg you are overweight or are taking medication that increases your oestrogen levels) you might be advised to make lifestyle changes that can restore the uterine lining. A follow-up biopsy should be taken to assess whether these changes have helped. The chance of the lining returning to normal in this scenario is 75%. (4)
If you have atypical endometrial hyperplasia, where cells are abnormal, you may be advised surgery to remove your uterus (hysterectomy) and possibly your ovaries due to their role in oestrogen production. If you are planning to have children, this is something that should factor into your decision-making and it may be that your initial treatment for endometrial hyperplasia is hormone-based (eg a form of progesterone).
Once endometrial hyperplasia has been successfully treated, it's important to have regular check-ins with your healthcare provider so that you can take action if it reoccurs.
Gynaecologist: If your GP suspects you have endometrial hyperplasia they may refer you to a gynaecologist for further investigations and treatment. You can avoid long waiting times by speaking directly to a gynaecologist through Bloomful.
Menopause specialist: If you are in perimenopause or menopause, speaking to a doctor who specialises in menopause can be helpful, particularly when it comes to monitoring lifestyle adjustments you need to make to address endometrial hyperplasia.
Fertility expert: If you plan on having children, speaking to a fertility specialist can help you understand the impact treatments will have on your fertility.
1. Don't ignore symptoms
If you notice changes to your menstrual cycle or experience any other symptoms, speak to your healthcare provider. Endometrial hyperplasia is a precancerous condition, which means that cells have the potential to develop into cancer if left untreated.
2. Know your risk factors
If you have any of the risk factors we mentioned above (eg diabetes, PCOS) let your GP/healthcare provider know, especially if you’re making a case for a gynaecology referral.
3. Treatments are tailored to type
Treatment approaches for endometrial hyperplasia vary depending on the type and severity of hyperplasia. Your healthcare team should make you aware of your type so that you can fully understand and assess your treatment options.
4. Consider your life stage
Depending on your age and family planning choices, you may need specialist support. For example, if you’re approaching or experiencing menopause, consulting with a menopause expert can offer specialised insights into managing endometrial hyperplasia within the context of hormonal changes and ageing.
References
(1). Incidence of endometrial hyperplasia (Published: 2009 Authors: Susan D. Reed, Katherine M. Newton, Walter L. Clinton et al)
(2). Endometrial Hyperplasia (Published: 2023 Authors: Gunjan Singh, Yana Puckett)
(3). Endometrial hyperplasia(Published: 2022 Author: Gloucestershire Hospitals NHS)
Care from the comfort of your home
When was the last time you felt truly heard by a healthcare professional?
At Bloomful, our clinicians listen deeply, ask the right questions, and commit to helping you overcome the health hurdles that are holding you back.
