⏱ 3 Min Read
Are hormones interfering with your sleep?
Words
Dr Louise Newson interviewed by Eleni Stefanou
Updated on
17 Jul 2024

About the expert
Dr Louise Newson is an award-winning doctor and educator. She is a member of the UK government’s menopause taskforce and the founder of the free Balance app for menopause support.
Dr Newson explains why hormone changes can wreak havoc on your sleep and how you can reclaim the night and safeguard your long-term health.
Why is it important to consider hormones when experiencing sleep disturbances?
Estrogen, progesterone and testosterone all have effects on our brain. They also impact other hormones in the brain, such as melatonin, and affect parts of the brain that help us sleep. So when these hormones fluctuate or are reduced, sleep can be a real problem.
What are some common hormonal reasons for sleep disturbances?
Often people struggle with anxiety. They might wake up in the night because they need a wee and then the anxiety takes hold preventing them from getting back to sleep. About 90% of women have PMS and PMDD, which presents similar symptoms of anxiety. So people might find that just before their period they experience sleep issues.
Something else to consider is that our hormone levels are at their lowest in the early hours of the morning. This can cause heart palpitations and heartburn, which can disturb sleep.
Contraception can also impact your nights. Testosterone is great for sleep, but the oral contraceptive pill can interfere with how well it works.
Does that level out at some point or can it have long-term effects, in which case you might recommend trying different contraception?
Absolutely. With any hormone treatment, whether it's HRT or contraception, you should always try it for three months - unless you're having a really difficult time - and then see if things change.
People tend to associate menopause with night sweats. Are we overlooking other sleep-related symptoms that could be a sign of perimenopause or menopause?
We surveyed nearly 6,000 perimenopausal and menopausal women and 79% reported sleep problems, while 68% reported vasomotor symptoms (hot flushes and night sweats). So a significant number of women are experiencing sleep disturbances without night sweats.
Yes, of course, if you have drenching night sweats you are going to wake up, but a lot of people wake up whether they have night sweats or not.
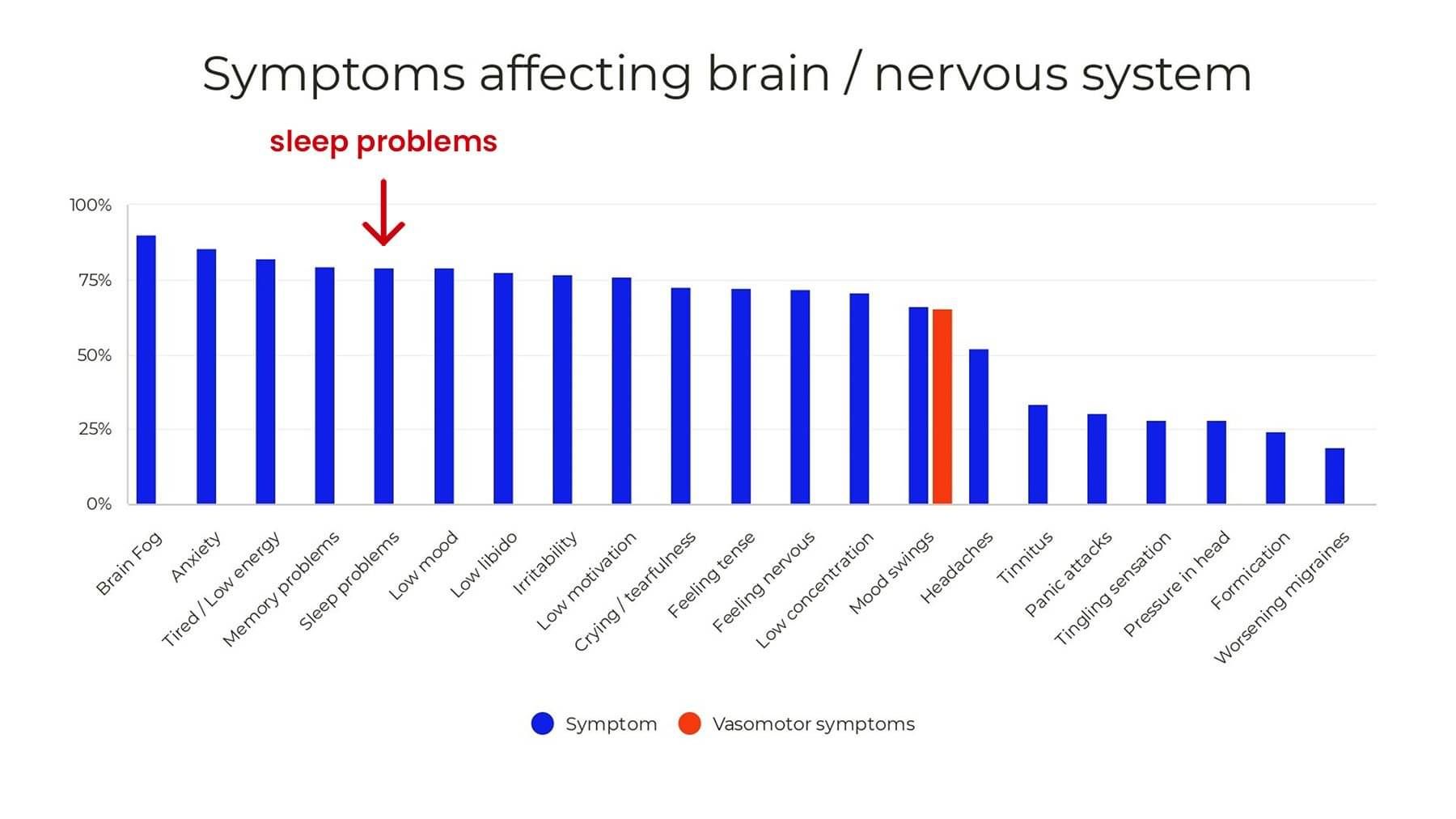
Data from 6,000 perimenopausal and menopausal women. Source: Newson Health
What are the best interventions for sleep disturbances?
If poor sleep is caused by fluctuating or low hormones, then hormone replacement therapy.
Obviously we need to be looking at whether there's a vitamin D or magnesium deficiency. Looking at exercise and how we manage our stress, whether we need to meditate. That should happen for anybody who doesn't sleep. But if we’re thinking about hormones, these interventions aren’t going to treat the underlying cause. If you had diabetes and were feeling tired because your glucose was high, you wouldn't not take insulin, would you?
Estrogen, progesterone and testosterone are thought of as sex hormones that control our periods but symptoms affect our brain more commonly than they do our genitourinary system.
How would you approach prescribing HRT specifically for sleep issues?
Often we start with a standard dose, depending on whether the person is perimenopausal or menopausal. We might take age into account as well. We’ll then review people and if there’s no improvement, then it’s about tailoring the dose for that individual.
We sometimes give progesterone because it’s very calming and good for sleep and we might add testosterone if needed. We might increase the dose of progesterone or change the form because having it orally or vaginally will have different effects.
How should people approach supplements? How do you make a decision about whether to take them and which ones will help with sleep?
It's really hard and very individual. Some people find that magnesium can be helpful. We recommend a supplement that combines different forms of magnesium and vitamin B to help with absorption. Sometimes we recommend a supplement called Serenity which contains magnesium and casein, a milk protein, which can help you feel more sleepy.
I would check iron levels, vitamin B12 and folate and if you’re deficient you might need to supplement. Everyone should be on vitamin D regardless of whether they sleep or not. But it's very individualised and the problem is a lot of people think, if I take a supplement, I don't have to eat as well, and in the longer term that’s not beneficial.
So I would balance hormones, look at nutrition and exercise, and add in supplements if needed, but I wouldn't go to them in the first instance.
Is there anything you'd like readers to be aware of that we haven't covered?
I recommend sleep tracking because a lot of younger women won’t be thinking about their hormones. If they're not sleeping well just before their period it's worth seeking help because we can give hormones for those few days when people are struggling with symptoms. It's really important that it's picked up.
I also think people don't see poor sleep as a problem. They think it's going to cause a bit of tiredness, but actually I see it as a chronic disease. I really worry about people that struggle with sleep. We know that chronic diseases and inflammation increase when people don't sleep.
We need to work out our own body clock and what works for us, which can take a while. Working out the best time to wind down, the best time to go to bed and being consistent. Because of my migraines, I go to bed at the same time every night. If I'm out even by an hour, it will trigger a migraine. So keeping a routine is really important when looking after our body and brain.