⏱ 3 Min Read
Why is sex painful for me?
Words
Dr Ashley Winter (as told to Eleni Stefanou)
Updated on
3 Apr 2024

About the expert
Dr Ashley Winter is a urologist and sexual health expert based in Los Angeles, California.
She walks us through the causes of painful sex and shares the questions she puts to patients to get to the root of the problem.
Foreplay matters
One of the first things I’m going to ask a patient is: what is your foreplay like? Even if there is absolutely nothing medical happening, if the person’s partner isn’t attentive to their needs and making sure they are adequately lubricated and prepared for sex, chances are they will experience discomfort and even pain.
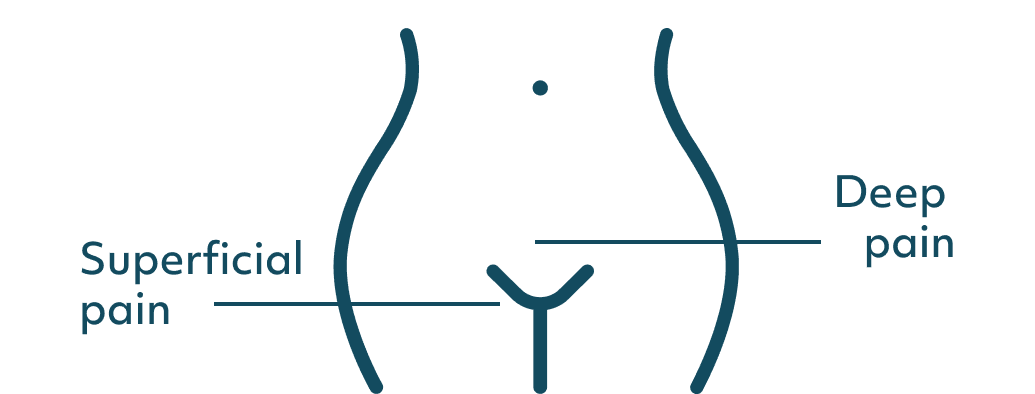
Pain types: deep vs superficial
I'm then going to ask whether the pain is deep or superficial because there is a difference between superficial dyspareunia (when pain is experienced at the vaginal opening or around the vulva) and deep dyspareunia, which is when the pain is situated deeper within the pelvis.
The surprising role of contraception
When it comes to superficial pain, it's important to determine if symptoms existed before starting contraception.
Let's say someone used a tampon when they were first menstruating at 13-14 and it wasn't painful. Let’s imagine that, aged 16, she was put on the oral contraceptive pill and started noticing some pain with insertion. One of my main hypotheses is going to be that she has something called hormone-mediated vestibulodynia, which is pain experienced in the hormone-sensitive tissue at the opening of the vagina, between the labia minora and the hymen.
Hormone impact
A common driver of this type of pain is a reduction in oestrogen and testosterone caused by contraceptive pills. A low-dose oral contraceptive pill can lower your oestrogen, while all combined oral contraceptives will reduce your testosterone. Low testosterone can also cause clitoral atrophy - when the clitoris gets smaller, impacting your ability to orgasm and experience pleasure during sex.
So many women are put on these medications before they become sexually active, so they don't have a baseline to say “Oh, this changed things.” They think that it's an innate part of their body.
Checking other meds
I also ask patients if they are on any other medications that might be impacting their hormones. For example, spironolactone, which is commonly used to treat acne, can further decrease testosterone levels when combined with contraception, potentially worsening their discomfort.

Easing the pain
If you experience superficial pain during sex, look up the type of contraception you are on and see whether it has an anti-androgen effect (meaning it impacts testosterone). If it does, try switching to a progestin-only pill or an IUD. Applying an oestrogen cream on the vulva can also help.
The menopause cause
Oestrogen declines dramatically in menopause, while levels will fluctuate during the years leading up to this moment (the perimenopause years). As we’ve seen, low oestrogen levels can make sex painful, so talking to your healthcare provider about using a topical oestrogen cream would be my key recommendation here.
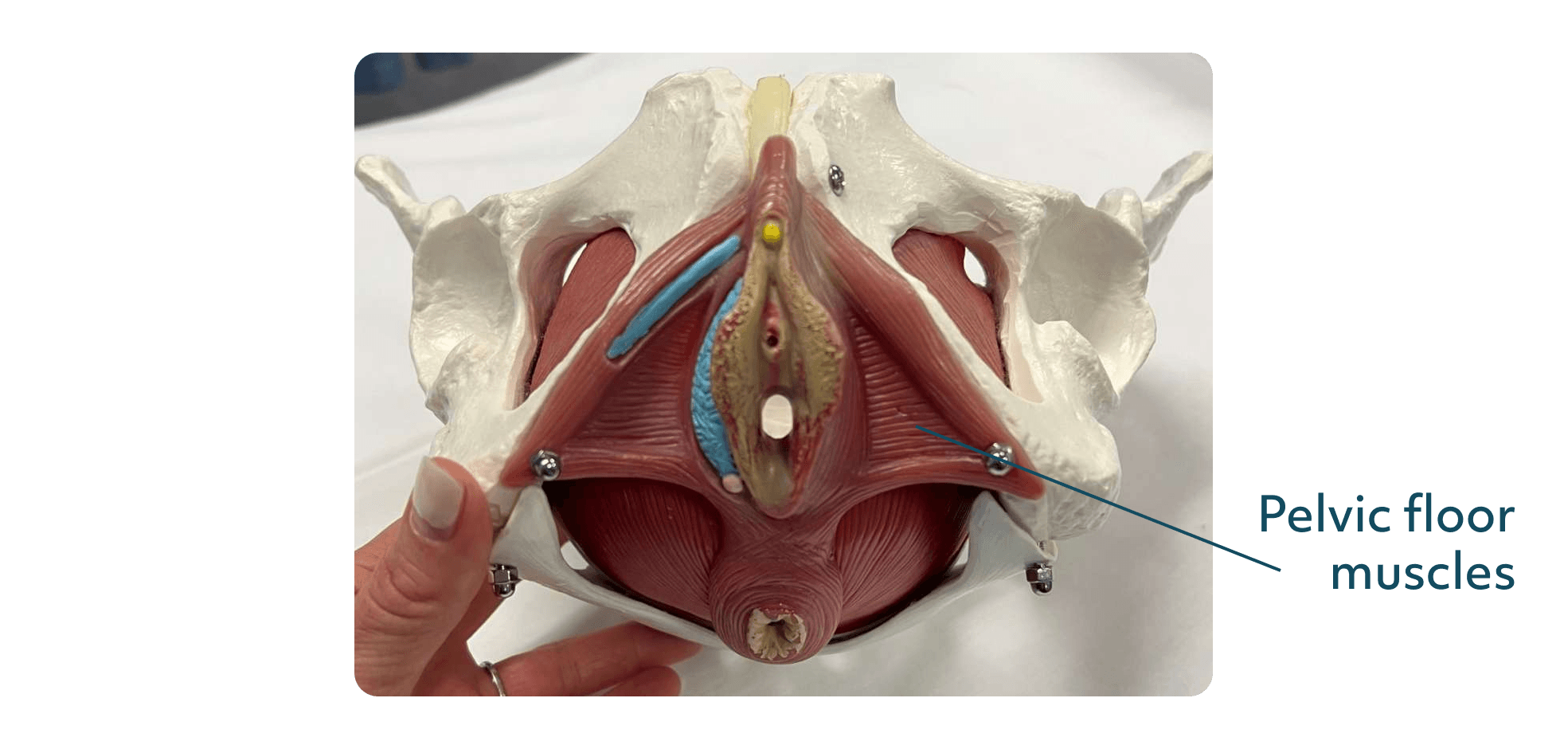
Muscular matters
Tight pelvic floor muscles are a common cause of painful sex. The medical term for this is vaginismus, but I don't love that word because it makes it sound like you have this histrionic vagina. The issue is in the muscles, not your vagina.
Your muscles are designed to tighten away from a painful stimulus. Think about it this way: if you touch something hot, your body automatically pulls away from it. So if the penis coming at you is the painful stimulus, you have designed yourself to tighten in preparation, and this can get worse when you’re not sexually active.
This is extremely common and telling someone to just relax is not a solution. Instead, you need to go to a pelvic floor therapist, who has many tools and resources that can help.
Physical abnormalities
Fibroids and endometriosis can also cause pain during sex. Endometriosis in particular can be associated with deep pain (although it can also cause superficial pain).
Keep a log of your symptoms in relation to your period. If pain presents or worsens during your period this could indicate you have endometriosis so talk to your doctor and advocate for an evaluation.
It’s also worth noting that, often with endometriosis, people are put on the combined oral contraceptive pill to improve their deep pain, but this can lead to superficial pain because the entrance to the vagina is so oestrogen-sensitive.
Infections
If the pain came on suddenly, it could be caused by an infection. Your healthcare provider can run a urine test or do vaginal swabs to check and, if needed, offer an appropriate treatment.
Don’t neglect the clitoris
I strongly advocate that women do a self-exam and look at their clitoris because it’s extremely unlikely that their healthcare provider will do this. You can pull the hood back and see if there’s inflammation and touch the area to see if it’s correlated with the pain.
Some women have clitoral phimosis, which is when the hood over the clitoris is fused or partially stuck. This can cause inflammation and pain when the clitoris enlarges with arousal.
Rare nerve condition
In rare cases, painful sex can be caused by something called neuroproliferative vestibulodynia, which is when there are too many nerve endings in the vestibule tissue (the opening of the vagina).
1. Focus on foreplay
Make room for foreplay so that you’re comfortable and adequately lubricated. Extending or changing up foreplay will also help your mind and body relax.
2. Profile your pain
Note down if your pain is deep, superficial or both. Log when the pain appears or worsens in your menstrual cycle. These details will help your healthcare provider investigate the source of the pain.
3. Consider your contraception
If you’re on contraception, check whether it has oestrogen or testosterone-lowering effects. If you think the pain you experience during sex could be related to these hormonal changes, talk to your healthcare provider about trying a different form of contraception (eg progestin-only pill or an IUD).
4. Support your pelvis
If you think your pain might be due to tightening muscles, it’s worth speaking to a pelvic floor specialist so that you can work with them to address the issue.
Care from the comfort of your home
When was the last time you felt truly heard by a healthcare professional?
At Bloomful, our clinicians listen deeply, ask the right questions, and commit to helping you overcome the health hurdles that are holding you back.
